There are a lot of misconceptions about the types of midwives who attend births in Utah including Southern Utah. Every woman has the right to know the credentials and skills of the midwife who may be attending her birth. Each type has it's positives and negatives. This video is a basic break down of the 4 different types of midwives to help you make the best choice for your family.
Friday, November 30, 2012
Tuesday, November 27, 2012
A Mothers' Story of a Planned Home Birth Turned Hospital Transport
The number one questions I get asked during a free consultation for my midwifery services is:
What happens if there is an emergency?
How do you get to the hospital?
How do you know you are getting there in time?I reassure the families that midwives are trained in dealing with normal birth. While we can handle a good majority of unforeseen complications at home we have keen eyes, the benefit of one-on-one individualized care, and intuition telling us when things might be safer in the hospital.
Most midwives have a 3-10% transport rate. The vast majority of these transports, I would go as far as to say 95% of them are non emergent transports.
Some examples on non-emergent transports in my practice might be:
Mother has a fever during labor
Mother's blood pressure is rising during labor
Mother is too exhausted to continue with her homebirth plan
There is unusual bleeding during the birth but mom and baby seem to be doing fine
After a long labor mother is not progressing and would like pain medication to see if it makes a difference
After pushing for many hours baby is not descending well into the pelvis
Baby's heart tones are not as reactive as they should be and may be too high or too low at some points
Baby has passed very thick meconium and giving us other warning signs that s/he may be in distress
Baby is born and there are obvious birth defects that many need further examination or baby might be showing signs of infection such as a temperature or fast breathing
Mother tore during the birth to the extent that she needs a surgeon to do extensive repair
In the case of a non-emergent transport in my practice the family and myself talk about all of the options. Based on our discussion and both of our intuitions we may make the choice that the birth may need to be moved to the hospital as it has become higher risk. I call the hospital and inform them that we are coming. The hospital is wonderful here and myself and my clients have always been treated with respect. They ask for information about the client so they can pull records and contact their OB if they have seen someone during their pregnancy or call the on-call doctor if not. We all load up in the largest vehicle we have and the baby and mother are monitored on the way to the hospital. The nurse copies my charts and the family checks in and the situation is assessed by the medical staff. I remain with the family the entire time they are at the hospital acting as their doula and support person as well as answering any questions the doctors and nurses might have.
The majority of non-emergent transports still end in vaginal and often even unmedicated births. A small minority end up with a cesarean for various reasons.
In the case of emergent transport I would handle the problem as well as possible at home while calling in an ambulance to transport the mother or baby to the hospital. I would still also call the hospital and tell them we were coming and what to expect. This is important! If you know that the mother needs a cesarean quickly it is crucial for your midwife to have a good relationship with the hospital so that their points of view regarding what is occurring is respected. It is not easy to call in a c-section team STAT but if your midwife has shown competence in the past the nurse on call will have no problem doing just that.
Some examples of emergent transport in my practice might be (keep in mind that each of these complications are very rare most with less than a 0.5% chance of happening during a birth with a full term newborn and healthy mother):
Prolapsed cord where the cord comes out before the baby -0.14% of births usually caused by artificially breaking your water or twins
Placenta Separating from the Uterine Wall before birth-01% of pregnancies world wide with poor nutrition and drug abuse the main cause
Uterine Rupture-0.07% of births with most of them being to women with twins, a transverse baby, or a previous uterine surgery such as a cesarean section
Postpartum Hemorrhage or greater than normal bleeding after birth-1.5% of all births. Using a midwife who is competent in herbal remedies to help stop bleeding as well as licensed so that they can legally provide I.V. therapy and anti-hemorrhagic medications such as pitocin reduces the need for transport for this reason
Fetal concerns such as trouble breathing- 10% of babies needs some assistance to breathe after birth which a qualified midwife is trained to handle at home and the baby breathes and the family stays at home. 1% of babies need extensive breathing support which would require transport
The families feelings about a transport are so important. How you feel about your birth is often more important that what actually happened at the birth.
I asked a past client of mine if she would be willing to share her story of a planned homebirth that ended in a hospital birth. She very selflessly agreed. Here is her story in her own words.
Please tell me about your choice to have a homebirth:
I had been interested in homebirth for a while. A local midwife had given a presentation on homebirth in one of my developmental psychology classes a couple of years before I got pregnant and I really liked what I heard. When I brought up homebirth to my husband after I got pregnant he said absolutely not. So, I started seeing a female OB. I knew I wanted a female doctor because I wanted someone who had experienced what I was going through and could anticipate my questions and calm my fears. After seeing her for almost 20 weeks, I decided that she was not the person I wanted to be with me at my birth. She never took the time to talk to me about any questions I had, nor did she make me feel calm or comfortable. I always felt like she was in a hurry to get somewhere else and I didn’t want to feel hurried during one of the most important events of my life. So I decided to change care providers to a family doctor. I chose this particular doctor because I had heard really great things about him from friends and family. My first visit was great. He was supportive of my desire to have a natural birth and he spent time with my husband and I never once making us feel like he was in a rush to get to his next patient. I was excited to have a doctor that I felt would be supportive of my decisions.
A few weeks after I switched doctors, my husband and I started taking DyAnna’s childbirth classes. One of my good friends had hired DyAnna to be her doula for her hospital birth and told me how amazing DyAnna was and that I should take her childbirth classes. During the six week course of classes, I realized again how much I wanted a homebirth. I decided that if I couldn’t have a homebirth I at least wanted DyAnna to be with me as my doula at the hospital.
When I was somewhere around thirty weeks, I was in for my doctors visit and he told me that was probably going to have to have a c-section because I was showing signs of pre-eclampsia. The “signs” he was referring to was that I had one episode of high blood pressure. Subsequent visits with him continuously got more negative. He never even pretended to remember me from visit to visit, he always asked if I was a new patient. He also made negative comments about my body while checking my baby’s heart tones. I left many appointments feeling embarrassed and ashamed. Since I was in my last trimester by then, I felt like it was too late to change care providers again. Then, at my last visit with him I gave him my birth plan. He read it and then told me that he was unwilling to follow it and that the things I wanted were unreasonable and crazy. The “crazy” and “unreasonable” things that I wanted were things like no deep suction, no vitamin k, no eye drops, and to delay clamping and cutting the cord. After telling me I was crazy, he again told me that I was borderline pre-eclamptic and that I was going to have to have a c-section. I was really upset after that visit and I immediately called DyAnna because I knew I could trust her to tell me what was really going on. She invited my husband and me to go visit with her and another midwife. We discussed the things that my doctor had said and they took my blood pressure and checked my urine. All of which were fine. There were no signs of pre-eclampsia. Then they asked if I would like to have a homebirth. I was ecstatic! It wasn’t too late to change care providers again and have a homebirth like I had originally wanted. This time my husband agreed since he had become much more educated about the safety of homebirth and we both knew we wanted these to amazing women to attend the birth of our child. We trusted them to tell us the truth at all times and I felt safe and comfortable with them.
What were some of your concerns going into your birth?
I was most concerned with the pain of labor. I had confidence that my midwives would take care of everything else. I knew they would be monitoring the baby and me so I wasn't concerned that anything bad would happen to us. I was only afraid of the unknown pain. Everyone told me that it was pain with a purpose and that made it easier to handle but that made no sense to me. Pain was pain right? Nope. Now, having gone through the pain of labor, I understand what pain with a purpose means and that makes it much more manageable.
How did your family react to your choice?
My family thought I was crazy. I’m sure they thought I was going to die. I come from a very medically oriented family. If you sneeze you take cold or allergy medicine. You have a sore throat you take antibiotics and go to the doctor and get tested for strep. They had a really hard time thinking that I wasn’t going to go to a doctor and that my baby wasn’t going to be born in a hospital. Some members of my family refused to talk to me about my plans for childbirth. Also it was suggested that I was letting others (meaning my midwives) make my decisions for me. It was really hard not to have the support I so desperately wanted from my family. But I was unwilling to sacrifice what I believed was best for me and my baby just to make my family happy. After my son was born, they still didn't want to have anything to do with homebirth or midwives. All I wanted to do was tell them how amazing my midwives were and what great support they had been and still were being but they wouldn't listen or let me talk to them about it. Now, over a year later they are fully supportive and have become more educated themselves about midwifery and homebirth.
How did your labor begin?
I was ten or twelve days over my estimated due date and I was miserable! I was huge and uncomfortable. Walking hurt, sitting hurt, standing hurt, and laying down hurt. My husband and I thought it would be a good idea to try to shake the baby out by taking our Jeep off-roading. Every bump would bring on a contraction and it would eventually get so painful that I would have to ask my husband to stop the Jeep so I could catch my breath. The bumps also made me have to pee so we were stopping the Jeep every five minutes so I could either climb out to take care of business or just catch my breath. My contractions would stop when the Jeep stopped so after an hour or so we gave up and went home. There were no more contractions. Since I was going to be pregnant forever I thought that there was no need to go to bed at a reasonable hour and I stayed up until 2:00 am watching old episodes of Lost. I finally decided to go to bed and just as my eyes started to close I felt a gush of fluid and my first real labor contraction began immediately after. So, I rolled out of bed, cleaned myself up and tried to not be excited because I knew I needed to sleep. Sleep turned out to be impossible because my contractions were coming every 3-5 minutes and they were hard. So we called our midwives and they headed over to our house. That was it! I was officially a woman in labor.
Was the beginning of your labor what you expected?
It was not. I didn’t expect my water to break before I had any real contractions. I also didn’t expect my contractions to be so hard and close together at the very beginning. I had no idea what to expect. I guess I sort of expected to never go in to labor! It was so exciting though. I was finally going to have my baby. It was an exciting and happy time. I wanted to call everyone that I knew and tell them that I was in labor and I was finally going to have my baby!
How were you treated by your birth team in early/active labor?
They were all wonderful! My husband was incredible. He was my rock throughout it all. My midwives were excited for me and were helping make me comfortable in any way that they could. I decided that I needed some things from the store and they were more than happy to run out and get whatever I needed. They were patient and loving and made me feel totally at ease.
What are some of your favorite memories about that time?
My favorite memory of early labor is everyone sitting together watching The Best of SNL Commercials. In particular I remember “I’m not a woman anymore, I’m a mom”. That was a lot of fun. My midwives were great. They were there for me when I needed them and they faded into the background when I didn’t. I wanted my husband to be near me at all times. I had thought that I wouldn’t want him touching me but it turned out that I wanted him next to me holding my hand or something the whole time. He was wonderful. He got in the birth tub with me even when he didn’t want to and was an active participant throughout my whole labor. He was there giving me sips of water and bites of food and helping me position myself to ease the pains of labor. I felt closer to him at that time than I ever had before. It was a time full of love and tenderness.
What tools did you use to cope with your labor pains?
Counter pressure on my lower back was a life-saver. At times it seemed to almost take the pain completely away. Water also helped. Being in the birth tub took all the pressure off my body and helped me to relax which, in turn, reduced the pain. I don’t remember doing much of anything else to help with pain. The counter pressure and the water were the two big ones. I suppose deep breathing and keeping my body relaxed helped also. Oh, I would also grab a body part of whoever was closest to me when a contraction started and squeeze as hard as I could until the contraction was over.
Tell me about when things changed in your labor and why you decided it would be better for your baby to be born at the hospital?
I’m not really sure. I guess I started to question whether or not my baby would be born at home when my midwives took turns checking my cervix and said that I just wasn’t dilating fully. They asked if they could try to help my cervix out and told me exactly what they would be doing and I agreed, but when they started it was just too painful and I asked them to stop. Of course, they immediately stopped but my concentration had been broken and I was no longer relaxed and the pain seemed to overwhelm me. I tried to tough it out for what seemed like hours but was probably not a very long time. I was determined to not wimp out though. I wanted a homebirth more than anything. I did not want to end up at the hospital because in my mind bad things happened had the hospital. I was technically fine and there was nothing wrong with my baby and I felt like I had no reason to go to the hospital. I think it was around 5:00 pm (my husband says it was only 3:00 pm) when my midwives said something like “It is okay to go to the hospital if you feel like you need to. No judgments.” I had known that all along, but having them say it out loud gave me the courage I needed to make the decision to go to the hospital. I don’t know that I ever thought it would be better for my baby to be born at the hospital but I felt like he just wasn’t going to come out at home. On top of that, I was in excruciating pain and there was no break between contractions. It was one on top of the other each one more painful than the last. And I still wasn’t fully dilated. So I asked to be taken to the hospital. Midwives Note used with permission: She had followed a wonderful labor pattern up to 9 cm but then had no change for over 4 hours with extensive non-typical pain and baby not engaging deeper into the pelvis.
How was the transport handled?
My midwives were amazing. The instant I said I wanted to go to the hospital they were making preparations. They called the hospital to let them know we were coming, they found me stuff to wear and helped get me presentable, and they got their van ready to go so all I had to do was be half carried to the car. I didn’t have to worry about anything and neither did my husband. They took care of everything.
Were you scared? What were you thinking of while going to the hospital?
No, I was in too much pain to be scared. All I could think about was the pain. There was no room for any other thoughts in my brain other than “It hurts! It hurts!”
How were you treated when you arrived at the hospital?
The hospital staff seemed to not know how to deal with a woman coming in who was in full blown labor. They tried to stick me in a wheelchair, which I know is protocol, but what woman who is dilated to a 9+ and having never ending contractions is going to be okay with sitting in a wheelchair? The poor girl with the wheelchair seemed to not know what to do when I refused to sit. I don’t remember much about what happened after we got to the room because of the pain, but I do remember that they were asking me endless questions that I didn’t know the answer to, nor did I care to answer them. It was really irritating to be asked stupid questions when I was clearly not in a state of mind to be answering them.
What did the doctor say about your reasons for going to the hospital and what course of action was taken?
I don’t remember what he said about my reasons for going. I just remember him giving me pitocin to try to make me fully dilate. I finally got an epidural and I have to say it was nice to be pain free. I think it was about an hour after being on pitocin that the doctor came back in and said that there had been no change. I told him that I wanted to continue to wait and see what would happen. Three hours later, after no changes with my cervix he came back in and told me I had two options. I could have a non-emergent c-section immediately or I could keep waiting until it became an emergency c-section. I was devastated. My beautiful, spiritual, and sweet homebirth had turned into a major abdominal surgery. After many tears, I decided to have the c-section sooner rather than later. I was terrified. I knew I needed to have my husband in with me during the surgery and I really wanted my midwives to be there with me also. I needed their support. They understood things better than I did and I wanted them to stay with me. I wanted my husband to be with our baby at all times and I knew that he would be leaving when they took our baby out while the doctor put me back together. I needed my midwives there with me to support me when my baby was taken away and my husband was gone. We were told that they would not be allowed in to surgery with me. I was really upset that they wouldn’t be able to come. My nurse who had barely spoken to me other than to ask me the stupid intake questions said “Don’t worry. I will be in there with you.” It was not comforting. I remember laughing to myself when my midwives responded to her statement with something like “She doesn’t know you so that’s not helpful.” It was nice to have them there to stand up for me.
When you went in for your cesarean what were you feeling?
I had a lot of emotions. I was scared and really really sad that I didn’t get to have the birth that I had been hoping for. I was also happy that I would get to see my baby soon. I was worried about being alone during the surgery since I had told my husband that he needed to be with our baby at all times.
Are there any details you would like to share about the surgery?
I remember that the nurse who told me she would be in there with me spent the whole time flirting with the doctor who was performing the c-section. She never said one word to me and the doctor only said things like “Tell me if you can feel this.” They were flirting and giggling the whole time! It was not how I imagined childbirth at all. The only person who actually spoke to me was my anesthesiologist. He was really nice. He asked me if I was nervous and explained what was going on and asked me questions about myself to help me relax. Midwives note: The official diagnosis was cord entanglement Cord was around the neck twice (which is not usually a problem) then around the chest and shoulder and around the abdomen and each leg preventing further descent into her pelvis.
When did you get to see your baby?
I saw him for about 10 seconds as they carried him out of the room. They didn’t show him to me or let me touch him though. I finally got to see him around thirty minutes after he was born and my surgery was finished and I was back in my room. But I was shaking so bad from the epidural that I couldn’t hold him.
Did you still feel supported by your midwives at the hospital?
Yes! They were incredible! Every time the doctor or a nurse said that I had to do something or they had to do something to me look for them to shake their heads no or nod yes. I had taken DyAnna’s childbirth classes and I had felt informed and knowledgeable about things that they hospital might want to do that are unnecessary but in the moment, I couldn’t remember anything so I needed them to help support me in my choices that I had already made but couldn't remember at the time especially when they went against the hospitals routine. They kept me entertained and did their best to keep me positive about the experience. They were also a huge support to my husband. After we got to the hospital he was able to shower and take a nap for a few hours. He told me he wouldn’t have felt safe or comfortable doing that without our midwives there to be with me. They stayed with me until after my baby was nursing and I felt comfortable enough for them to leave. They came back to the hospital to check on us the next day also.
How was your nursing experience at the hospital?
That first night it was fine. My midwives were there and helped me get everything figured out. My baby had no latching problems and everything was going well. The next day, a lactation consultant showed up and asked how things were going. I said we were fine and didn’t need any help. She insisted that we did, then she reached out and grabbed my breast and started squeezing it. Then, she began smashing my baby’s face into it. I am a very private person and she was up in my very personal space doing things that I didn’t want done after I had told her I didn’t want help. It was a horrible experience. I was used to my midwives gentle touch and they always asked and waited for permission before they touched me anywhere. On top of the awful lactation consultant I had hospital staff coming in and out of the room messing with my IV and trying to talk to me and whatever else they do while I was trying to nurse. All I wanted was to nurse my baby in peace without being exposed to everyone under the sun. Overall I hated trying to nurse my baby at the hospital.
When did you go home?
I went home two days after the c-section. It was a horrible transition from the hospital to home. First off, could barely stand upright and walk much less do anything else like carry my baby. After spending the first couple days of my baby’s life in the hospital it seemed unnatural to be caring for him at home. I sort of felt like “What do I do now?” While the transition to motherhood can be strange for homebirthing women as well, I am positive it is a much more strange experience for women who have to bring their babies home from the hospital. Birthing at home naturally leads into motherhood. Bringing a baby home from the hospital is not.
Did your midwives clean up the homebirth supplies before you got home?
Of course they did! They even fed our cat since we were in such a hurry to get to the hospital we hadn’t even thought about it. When I got home from the hospital there was no sign that they had even been there. Our house was spotless.
How was your experience physically once you got home?
It was really hard to do anything. I couldn’t lay flat so sleeping was difficult, I couldn’t bathe myself or do any other basic self-care. I could barely dress myself. It is impossible to recover from a major surgery and care for a newborn at the same time. My poor husband had to do everything for us. I was so tired because I wasn’t sleeping well and I thought I was going to go crazy not being able to do anything for myself.
Did you feel supported by your midwives postpartum?
Again, they were amazing! I saw them many times after my baby was born. Our first visits were in the hospital and in my home then, when I was more mobile, our visits were in one of their homes. I saw them at least ten times the first six weeks of my baby’s life. They cared about how I was doing physically, spiritually and psychologically. In contrast, I saw the Obstetrician who did the c-section two times in the same six week period and he only cared about how my incision was healing not about how I was doing psychologically.
At one point, I started having panic attacks from lack of sleep and some other things. My midwives came over immediately and offered their support. They talked to me about my concerns and shared their own experiences and offered to help in any way they could. They even offered to come stay with my baby so I could get some much needed sleep. I wouldn’t have trusted him to anyone else during that period. I also called and texted them many times throughout the first few months of my son’s life. They were always happy to answer any questions or concerns that I had. I have no words to express how grateful I am to them for being so supportive and loving during that time. They are wonderful women. And I love them!
How did you feel about the transport?
While It wasn’t my dream childbirth experience, I was mostly just happy that my baby was safe and healthy and so was I. I wished I hadn’t had to go to the hospital, but I couldn’t see how anything could have been different. We tried our best to have a homebirth and it just didn’t work out. I was disappointed, but that didn’t outweigh the joy of having a beautiful healthy baby.
How do you feel about your overall experience 18 months later?
A few months ago I went through a period where I was really angry that I had to go to the hospital. I felt like there was something wrong with me and I was feeling down in the dumps spiritually. I was feeling like if I had been more righteous, prayed harder, and had more faith then I wouldn’t have had to go to the hospital. I talked to my husband about my feelings and he helped me understand again that we actually were blessed during that time. Our son had been born and he was perfect. He was always fine and so was I. We don’t always get what we want and we need to be thankful for the blessings we have been given. Now, looking back at all that we went through it was such a good bonding experience for my husband and me. We are closer than we were before all this happened and I still feel like I had a homebirth.
How do you feel about homebirth after your experience?
I am passionate about homebirth. It is such an empowering experience. It is also beautiful, spiritual, and gentle which are things that I don’t associate with hospital birth. I hope to have my future children at home. While I admit that the hospital can provide necessary life-saving options, I don’t believe that all women need the hospital for childbirth. I love the experience I had at home with my midwives. And I wish that all women could have that same experience.
Monday, November 26, 2012
I Had a Baby and Things are Different "Down There"
You had a beautiful vaginal birth the way that babies were made to be born but now it is a few months later and you noticed things "down there" do not seem quite the way they used to.

Following, you will see an explanation of what might be going on that is different and what if anything you need to do. Keep in mind most change is normal and requires nothing different.
Scar Tissue
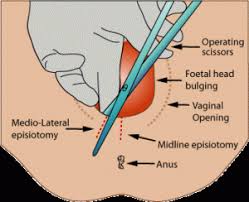
What it looks like-There is a line from between your vagina to your rectum.
Where it came from-If you had an episiotomy or tore significantly and needed stitches you may have a line of scar tissue on your perineum. Usually this is painless and does not cause any problems.
What you can do to help- If it is painful or in preparation for subsequent births where hopefully you will not tear you may want to apply some evening primrose and coconut oil daily and rub it into the scar tissue.
Extra Flaps of Labial Skin
What it looks like- The folds in your labia (the lips) look different and may have extra folds or flaps.
Where it came from- As the skin stretches it usually goes back to its original shape but not always and occasionally there may be slight tears which cause extra pieces of skin.
What you can do to help- Most of these are not painful and are cosmetic only. You may be surprised that intercourse after a baby feels better because of this extra skin. If that is not the case and it is painful talk to a gynecologist about having them surgically removed.
Cystocele

What it looks like- A ball like lump of tissue on the top part of your vaginal canal.
Where it came from- A cystocele is a medical condition that occurs when the tough fibrous wall between a woman's bladder and her vagina (the pubovesical fascia) is torn by childbirth, allowing the bladder to poke down into the vagina. Even if you have a c-section you can still get a cystocele just by being pregnant.
What you can do to help- For most women a cystocele causes no problems. In some cases the woman may need to urinate more frequently Occasionally it may cause problems with retaining or leaking urine or pain during intercourse. Some things you can do to help your cystocele heal are: maintain a healthy weight, avoid lifting things that are very heavy, urinate frequently to keep your bladder empty, space your pregnancies to allow healing time between each child, avoid strenuous running that puts pressure on the bladder. If it is very severe there is a surgical procedure that can be performed by and gynecologist.
Rectocele

What it looks like- A ball like lump of tissue on the bottom part of your vaginal canal.
Where it came from- A rectocele results from a tear in the rectovaginal septum (which is normally a tough, fibrous, sheet-like divider between the rectum and vagina). Rectal tissue bulges through this tear and into the vagina as a hernia. There are two main causes of this tear: childbirth, and hysterectomy. Women who have birthed a posterior baby, face up, are more likely to have a rectocele,
What you can do to help- For most women a rectocele causes no problem. In some cases a woman may have a "full" feeling in their vagina, have trouble having a bowel movement or have discomfort during intercourse. Eating a high fiber diet and encouraging regular bowel movements is the best treatment. Using a stool to place your feet on and avoid bearing down while passing stool helps a lot. If you are having major pain or problems a gynecologist can perform a surgery to repair things.
Vaginal Prolapse

What it looks like- Extra tissue in your vagina, a feeling of "falling out", feeling your cervix (entrance to your uterus that feels like the tip of your nose) just inside your vagina, vaginal wall hanging out of your vagina.
Where it came from-Vaginal prolapse is characterized by a portion of the vaginal canal protruding (prolapsing) from the opening of the vagina. The condition usually occurs when the pelvic floor collapses as a result of childbirth. Childbirth with an epidural, a very large baby or pushing for a very long time increases your chances of prolapse.
What you can do to help- Give yourself time as things tend to heal by themselves. Avoid lifting heavy object or running and jumping. If it is problematic a gynecologist can prescribe a pessary, which is a plastic rod that you wear internally to hold everything in, or perform surgery to repair things.
What about Kegel exercises?
Kegel exercises can help to strengthen the pelvic floor muscles and for years they were thought to be the cure all for all pelvic floor issues.
All about Kegel Exercises
New studies have shown that doing sets of squats several times per day are actually far superior to Kegel Exercises.
All about squats for pelvic floor health
In the end remember that "down there" is beautiful no mater what has changed since you gave birth to your baby. If it is just cosmetic think of it as ever evolving if it is painful or problematic consider some of the above options to improve your quality of life.

Scar Tissue
Where it came from-If you had an episiotomy or tore significantly and needed stitches you may have a line of scar tissue on your perineum. Usually this is painless and does not cause any problems.
What you can do to help- If it is painful or in preparation for subsequent births where hopefully you will not tear you may want to apply some evening primrose and coconut oil daily and rub it into the scar tissue.
Extra Flaps of Labial Skin
What it looks like- The folds in your labia (the lips) look different and may have extra folds or flaps.
Where it came from- As the skin stretches it usually goes back to its original shape but not always and occasionally there may be slight tears which cause extra pieces of skin.
What you can do to help- Most of these are not painful and are cosmetic only. You may be surprised that intercourse after a baby feels better because of this extra skin. If that is not the case and it is painful talk to a gynecologist about having them surgically removed.
Cystocele

Where it came from- A cystocele is a medical condition that occurs when the tough fibrous wall between a woman's bladder and her vagina (the pubovesical fascia) is torn by childbirth, allowing the bladder to poke down into the vagina. Even if you have a c-section you can still get a cystocele just by being pregnant.
What you can do to help- For most women a cystocele causes no problems. In some cases the woman may need to urinate more frequently Occasionally it may cause problems with retaining or leaking urine or pain during intercourse. Some things you can do to help your cystocele heal are: maintain a healthy weight, avoid lifting things that are very heavy, urinate frequently to keep your bladder empty, space your pregnancies to allow healing time between each child, avoid strenuous running that puts pressure on the bladder. If it is very severe there is a surgical procedure that can be performed by and gynecologist.
Rectocele

Where it came from- A rectocele results from a tear in the rectovaginal septum (which is normally a tough, fibrous, sheet-like divider between the rectum and vagina). Rectal tissue bulges through this tear and into the vagina as a hernia. There are two main causes of this tear: childbirth, and hysterectomy. Women who have birthed a posterior baby, face up, are more likely to have a rectocele,
What you can do to help- For most women a rectocele causes no problem. In some cases a woman may have a "full" feeling in their vagina, have trouble having a bowel movement or have discomfort during intercourse. Eating a high fiber diet and encouraging regular bowel movements is the best treatment. Using a stool to place your feet on and avoid bearing down while passing stool helps a lot. If you are having major pain or problems a gynecologist can perform a surgery to repair things.
Vaginal Prolapse

Where it came from-Vaginal prolapse is characterized by a portion of the vaginal canal protruding (prolapsing) from the opening of the vagina. The condition usually occurs when the pelvic floor collapses as a result of childbirth. Childbirth with an epidural, a very large baby or pushing for a very long time increases your chances of prolapse.
What you can do to help- Give yourself time as things tend to heal by themselves. Avoid lifting heavy object or running and jumping. If it is problematic a gynecologist can prescribe a pessary, which is a plastic rod that you wear internally to hold everything in, or perform surgery to repair things.
What about Kegel exercises?
Kegel exercises can help to strengthen the pelvic floor muscles and for years they were thought to be the cure all for all pelvic floor issues.
All about Kegel Exercises
New studies have shown that doing sets of squats several times per day are actually far superior to Kegel Exercises.
All about squats for pelvic floor health
In the end remember that "down there" is beautiful no mater what has changed since you gave birth to your baby. If it is just cosmetic think of it as ever evolving if it is painful or problematic consider some of the above options to improve your quality of life.
Wednesday, November 14, 2012
A Siblings Memory of Birth 3 Years Later
All three of my older children ages 6,4 and 2 were present at the birth of my last baby 3 years ago. I prepared them with easy discussion about birth and had them watch a few birth videos to be prepared for the fluids and sounds. When the time came I still wanted them there. As typical for my labor pattern he was born mid morning. I wondered what the long term memories would be for my children as they were so young when Oliver was born. I was pleasantly surprised by what memories she had.

This is what my daughter age 6 at the time remembers from the birth written in her own words.
What I remember about my baby brother Oliver’s birth is waking up when it was still dark, that is very strange for me because I am usually a sleep in late. I crept up stairs to go cuddle with my mom. When I looked in her room she was not there so I went back to bed.
After a few hours I went back up the stairs to see where my parents where. I found them in the bathroom surrounded in people I knew as midwives and doulas such as Ms. Hopper, a friend of my mothers and a mother of one of my many friends who is also midwife and Ms. Janet, a friend of my mothers and a mother of one of my many friends who is also a doula. There was also someone there taking pictures.
My mother was in the bathtub and she explained that the baby was coming out. She would close her eyes when she felt some pain and then would talk to me and everyone else in the room in between. I was just about as excited as a six year old could be without exploding! I had heard quite a few things about this baby. My third brother, finally coming although I didn't know he was a boy at the time! I mean what could be more exciting than that?!
As always the birth took forever but I amused myself with drawing a picture of what I hoped my younger sibling would look like. I also came up with a list of names that I liked for the baby. While I did that my other two brothers where busy watching a movie upstairs. When it was actually time for the baby to come out my brothers ran into the room just in time to see my mom and dad catch my baby brother in the bath tub. I couldn't see much because he was born in the water. He cried and cried after they put him on my mom's chest. He was so cute.
Another thing I was excited about was the fact that my mother said I could snip the umbilical cord! After having two brothers I wanted a baby sister but that didn't happen.
When Oliver finally came out of the tub out we wrapped him in a red towel. I sat on the bed with my mom holding my new brother and watched the midwife do an examination of the baby to make sure he was healthy. I loved watching him nurse he looked so happy.
So sweet and so perfect. I am so glad she got to be there for that special event.
Monday, November 12, 2012
13 Ways to Keep Your Newborn Cold and Flu Free this Winter
With the Holidays often come colds and flues. The last thing you want to deal with is an ill newborn or infant. Consider these 13 tips to keep your newborn healthy. After all you birthed your baby at home to avoid exposure to hospital super bugs lets keep her healthy.
1. Exclusively breastfeed. Hint: exclusively means only milk no solid food. Exclusively breastfeed for a minimum of 6 months and continue nursing into your babies toddlerhood. The same antibodies and amazing nutrients your breastmilk has when your baby is a newborn is still helpful when your baby is 13 months old. Breastfeeding is also insurance through an illness that your baby is still getting some good qulaity nutrition even if they are vomiting or don't have much of an appetite.

2. Wear your baby. Keeping your baby close to you limits other people exposing their germs to your baby. A person is also much less likely to touch your baby if your baby's head it two inches away from your breast.

3. Keep your baby dressed warmly but not too warmly. Overheating is as difficult on your babies immunity and physical well being and being too cold. Your newborn and young infant will be comfortable in one more layer than you are. So if you are wearing long sleeves and pants consider putting the same on your baby plus a little hat or socks as well.

4.Wash your hands. No one touches your baby more than you do. Wash your hands frequently and if your child is old enough to touch anything wash their hands as well.

5.Avoid public places. Sounds cliche but most people do not know they are sick until it is too late. Restaurants and Christmas parties and germ cities. Keep your baby away from others at parties and if someone feels they absolutely must touch your baby have them touch their toes not their faces or hands.

6. Avoid letting baby touch these 6 germ magnets
* Bed linens of someone who is ill
* Bathtubs
* Shopping cart handles
* Playgrounds
* Carpets
* Kitchen Sink

6. Go outside away from recirculated air and allow the sun to hit their skin. Vitamin D from sunlight is a top immunity booster.

10. Ditch the pacifier. I never encourage the use of pacifiers but if your baby needs one consider stopping after 6 months when the babies biological need to suck goes down significantly. As hard as we try it is difficult to keep pacifiers clean and free from germs.

12. Avoid well baby visits. If you are planning on not immunizing and don't have any exact concerns you want the doctor to address avoid well baby visits because it exposes the baby to an entire room of sick children.

13. Say no to antibiotics- most illnesses are viruses and antibiotics does no good. Consider using probiotics to build your baby's immunity instead by filling his gut with germ fighting positive bacteria. Breastmilk naturally contains probiotics but you can also give your baby additional powdered probiotics.

1. Exclusively breastfeed. Hint: exclusively means only milk no solid food. Exclusively breastfeed for a minimum of 6 months and continue nursing into your babies toddlerhood. The same antibodies and amazing nutrients your breastmilk has when your baby is a newborn is still helpful when your baby is 13 months old. Breastfeeding is also insurance through an illness that your baby is still getting some good qulaity nutrition even if they are vomiting or don't have much of an appetite.
2. Wear your baby. Keeping your baby close to you limits other people exposing their germs to your baby. A person is also much less likely to touch your baby if your baby's head it two inches away from your breast.
3. Keep your baby dressed warmly but not too warmly. Overheating is as difficult on your babies immunity and physical well being and being too cold. Your newborn and young infant will be comfortable in one more layer than you are. So if you are wearing long sleeves and pants consider putting the same on your baby plus a little hat or socks as well.

4.Wash your hands. No one touches your baby more than you do. Wash your hands frequently and if your child is old enough to touch anything wash their hands as well.

5.Avoid public places. Sounds cliche but most people do not know they are sick until it is too late. Restaurants and Christmas parties and germ cities. Keep your baby away from others at parties and if someone feels they absolutely must touch your baby have them touch their toes not their faces or hands.
6. Avoid letting baby touch these 6 germ magnets
* Bed linens of someone who is ill
* Bathtubs
* Shopping cart handles
* Playgrounds
* Carpets
* Kitchen Sink
6. Go outside away from recirculated air and allow the sun to hit their skin. Vitamin D from sunlight is a top immunity booster.

10. Ditch the pacifier. I never encourage the use of pacifiers but if your baby needs one consider stopping after 6 months when the babies biological need to suck goes down significantly. As hard as we try it is difficult to keep pacifiers clean and free from germs.
12. Avoid well baby visits. If you are planning on not immunizing and don't have any exact concerns you want the doctor to address avoid well baby visits because it exposes the baby to an entire room of sick children.
13. Say no to antibiotics- most illnesses are viruses and antibiotics does no good. Consider using probiotics to build your baby's immunity instead by filling his gut with germ fighting positive bacteria. Breastmilk naturally contains probiotics but you can also give your baby additional powdered probiotics.
Friday, November 9, 2012
Utah Baby Names
Choosing what to name your child is very important. Most parents don't want to choose something so unusual that no one can pronounce the child's name, but they also don't want their child to be one of 3 other children in their class with the same name. The web has a lot of great resources to help you choose the best name for your Utah baby. I have many options and ideas listed here on my website.
Many Utah parents when naming their baby's get very creative in both the name and the spelling. I came across this today and thought it was good for a laugh.
Many Utah parents when naming their baby's get very creative in both the name and the spelling. I came across this today and thought it was good for a laugh.
Wednesday, November 7, 2012
Children Appropriate Youtube Video's of Birth
All three of my older children chose to attend the homebirth of their youngest brother three years ago. We did some preparation and had care givers around to care for them if they wanted to leave. It was a very positive experience with my daughter who was 7 cutting the cord, my son who was 4 announcing the gender and my 2 year old son showing us how to dress out new baby by dressing his baby doll.
I try not to post mostly original content however I really think this blogger did an excellent job of finding and classifying youtube videos that would be appropriate for children at different levels. Enjoy!
Video's to prepare children for childbirth.
I try not to post mostly original content however I really think this blogger did an excellent job of finding and classifying youtube videos that would be appropriate for children at different levels. Enjoy!
Video's to prepare children for childbirth.
Sunday, November 4, 2012
What is the Difference Between a Birth Center and Birth Suite and a Home Birth in Utah?
I get asked this question all the time
What is a birth center in Utah?
A birth center in Utah is almost always staffed by Certified Nurse Midwives. The birth center must be in near proximity to a hospital. It needs to be constructed adequately to provide emergency service (rolling beds etc.) to move through out it. They are required by law to mandate certain laboratory tests for both mother and baby and must carry liability insurance as well as malpractice insurance which is where a large amount of your birth fee goes. All nursing services provided at the center must be done by licensed nurses. There can be up to five birthing rooms at a birth center. There are restrictions on what pregnant women may birth in a birth center example: no twins. Epidural anesthesia or cesarean births are not performed at a birth center. Here is a list of birth center laws for Utah. There is only one free standing birth center in Utah and it is located in Salt Lake City. Because of all of the additional fees and laws many birth centers do not stay in business for long. The average length of stay after a birth at a birth center is 4-8 hours.
What is a birth suite in Utah?
A birth suite it essentially a designated birth space for an out of hospital birth. All of the same equipment that your midwife offers at a homebirth is also available for those who want to birth in a birth suite. There is no difference in equipment offered. There may only be one birthing room in a birthing suite. Midwives and clients may determine their own qualifications for birthing at a birthing suite so depending on your midwife that may include birthing twins, breeches, etc. Birth suites are not required to be with in a prescribed distance from a hospital. Any type of Utah midwife, Traditional, Direct Entry, CPM, Licensed or CNM, can work at a birth suite. Some medical options may be available depending on your midwifes legal stance such as I.V. therapy, antibiotics in labor, and pitocin for postpartum hemorrhage. No epidural anesthesia or cesarean births are performed at a birth suite.The average length of stay after a birth suite birth is 4-8 hours.
Why would someone want to birth at a birth suite (birth center birth is not an option in Southern Utah)?
Some people are uncomfortable at the thought of birthing in their homes. They may be living in a space that in noncondusive to a private birth such as living with relatives or worry about sound traveling through apartment walls. They may have a belief that birth is safer out of the home. They may have family and friends who are less concerned about a birth suite/center birth than a home birth. They may have a young family and want some time alone with the baby after the birth before returning to regular child care.
I provide birth suite care at two different facilities one birth suite in St. George Utah and the other birth suite in Cedar City Utah. I am a private independant contractor with permission to use the facility for an additional facility fee. If you feel like a birth suite birth might fit your families needs give me a call at -435-215-6514 or email me at completebeginnings@gmail.com
"What is the difference between a home birth and birth suite or birth center birth?"First we need to look at the difference between a birth center and birth suite.
What is a birth center in Utah?
A birth center in Utah is almost always staffed by Certified Nurse Midwives. The birth center must be in near proximity to a hospital. It needs to be constructed adequately to provide emergency service (rolling beds etc.) to move through out it. They are required by law to mandate certain laboratory tests for both mother and baby and must carry liability insurance as well as malpractice insurance which is where a large amount of your birth fee goes. All nursing services provided at the center must be done by licensed nurses. There can be up to five birthing rooms at a birth center. There are restrictions on what pregnant women may birth in a birth center example: no twins. Epidural anesthesia or cesarean births are not performed at a birth center. Here is a list of birth center laws for Utah. There is only one free standing birth center in Utah and it is located in Salt Lake City. Because of all of the additional fees and laws many birth centers do not stay in business for long. The average length of stay after a birth at a birth center is 4-8 hours.
What is a birth suite in Utah?
A birth suite it essentially a designated birth space for an out of hospital birth. All of the same equipment that your midwife offers at a homebirth is also available for those who want to birth in a birth suite. There is no difference in equipment offered. There may only be one birthing room in a birthing suite. Midwives and clients may determine their own qualifications for birthing at a birthing suite so depending on your midwife that may include birthing twins, breeches, etc. Birth suites are not required to be with in a prescribed distance from a hospital. Any type of Utah midwife, Traditional, Direct Entry, CPM, Licensed or CNM, can work at a birth suite. Some medical options may be available depending on your midwifes legal stance such as I.V. therapy, antibiotics in labor, and pitocin for postpartum hemorrhage. No epidural anesthesia or cesarean births are performed at a birth suite.The average length of stay after a birth suite birth is 4-8 hours.
Why would someone want to birth at a birth suite (birth center birth is not an option in Southern Utah)?
Some people are uncomfortable at the thought of birthing in their homes. They may be living in a space that in noncondusive to a private birth such as living with relatives or worry about sound traveling through apartment walls. They may have a belief that birth is safer out of the home. They may have family and friends who are less concerned about a birth suite/center birth than a home birth. They may have a young family and want some time alone with the baby after the birth before returning to regular child care.
I provide birth suite care at two different facilities one birth suite in St. George Utah and the other birth suite in Cedar City Utah. I am a private independant contractor with permission to use the facility for an additional facility fee. If you feel like a birth suite birth might fit your families needs give me a call at -435-215-6514 or email me at completebeginnings@gmail.com
Saturday, November 3, 2012
How Many Hours to Become a Homebirth Midwife?

I came to my midwifery journey in a round about basis. I can't say that I always knew I would be a midwife but my life experiences have definitely helped bring me to this place. I looked into becoming a Certified Nurse Midwife briefly while on I was on the nursing track. After the birth of my second in 2005 I looked at different distance education options including Midwifery College of Utah and National College of Midwifery. My midwife for my second offered to be my preceptor if I went with a school she was familiar with. I also looked into finishing my nursing degree and then doing my CNM through Frontier School of Midwifery which would be relatively easy since I already had a Bachelors of Science Degree. In the end we moved away and I resolved myself not to do midwifery or other birth work. We moved to an area that had no CNM's or licensed midwives that did home births. I was very grossly misinformed regarding the education it took to become a traditional midwife and thought I would never want to train with any of the midwives locally.
I took a little over a year off. Few people even knew I had ever been involved with birth work and it was a much needed break. After the difficult birth of my third I knew that in order to be sure that quality midwifery care was offered in the area I would need to help by providing it myself so my midwifery journey began. I attended a few births of mutual friends with a local midwife I had been friends with for a few years. We hit it off and before I knew it I had transitioned from assistant to apprentice.
I still struggled about whether or not I needed a more traditional school. In the end it came down to a few things. 1- I had already done the traditional college route and done it well graduating with and A- average and learned and retained very little compared to the amount of time spent. 2- Money. We already have so much student loan debt for my husbands law degree that the thought of spending more money on my school for a career that wasn't a huge money maker just wasn't possible for my family. 3- I wanted to be able to tailor what I learned and avoid the busy work. I eventually developed my own curriculum and study system and passed the NARM exam on the first time with flying colors.
It took me a little over 3 1/2 years to complete all of the things needed to sit for the NARM (I had more than enough numbers and experience a year earlier but I had some documentation problems) and then an additional 6 months of waiting for the next exam. For those years of my life I spent time studying individually, studying and discussing with my preceptor, teaching childbirth classes, attending doula births, attending prenatals, births, and postpartum visits, doing skills classes, attending workshops, and forming and attending a local and several online study groups.
In the end the time spent in my apprenticeship ended up looking something like this:
Time spent studying individually, reading, writing protocols etc.
8 hrs a week x 208 weeks =1664 hours
Time spent doing prenatals and postpartum visits
6 hrs a week x 208 = 1248 hours
Time spent in skills class (suturing practice, exams, etc.)
5 hrs a month x 48 months = 240 hours
Discussion, review and study with my preceptor
2 hrs a week x 208 = 416 hours
Birth attendance
2 births a month at an average of 8 hours per birth x 48 months = 768 hours
Additional workshops
24 hours total
Study Groups
2 hours a week x 52 weeks x 48 months = 416 hours
Childbirth classes and doula births
3 series a year at 18 hours per series plus another 20 hours a year doing doula births x 4 years =296
Total: 5072 hours of study and instruction
Approximate cost for books, workshops, gas, food, childcare and supplies $12,000
NARM the national midwifery association that provides the test for your Certified Professional Midwife required a minimum of 1350 hours.
Community School of Midwifery
Midwifery School
I went through quite the ordeal in order for me to sit for the national NARM exam and finally receive my Certified Professional Midwife credential. I did self study and had much hands on support from my preceptors but little help with book learning. I vowed to do everything I could to make it easier for all my midwifery sisters who came after me. I was asked to join this amazing midwifery school and assist them as the Academic Dean. I am both humbled and excited by the opportunity. The school provided weekly in person education for midwifery students at several Utah locations.
Please visit http://www.thecommunitymidwife.com/ for more details.

Labels:
Apprentice,
Breastfeeding,
Childbirth,
Childbirth Education,
Childbirth. Certification,
CPM,
Doula,
Goals,
International Service,
Midwfery Student,
Midwife Sisters,
Motherhood,
NARM Exam,
Student
St. George Magazine Article July 2012
What can you do during
your 20’s and 30’s to reduce your Chances of Breast Cancer?
According
to the Centers for Disease Control and Prevention, breast cancer is the second
most commonly diagnosed cancer among American women. Less than 0.5 percent of women
will get breast cancer before age 39. Your 20’s and 30’s are prime time for
preventative measures to help keep your risk as low as possible continuing into
your 40’s and beyond. Here are things you can control to help keep your risk
low:
- Maintain a healthy weight. Staying trim doesn't just look good-it helps reduce your risk of breast cancer. Excess fat can increase the amount of estrogen your body produces which can increase your chances of breast cancer.
- Watch your alcohol intake to no more than one drink per day. Three drinks per day increases your rate by 50%
- Consider avoiding soy. There is conflicting evidence about whether soy increases your chances of breast cancer due to its pseudo-estrogenic effect. It might be better just to avoid it until we know more.
- Consider a non- hormonal birth control method. The available data about hormonal contraceptives containing estrogen, suggests a slightly increased risk, so consider whether the benefits of the pill outweigh the risk of taking it. If you have a family history of breast cancer, for example, you may want to choose a different form of birth control.
- Have a baby if that is something you would like to do. Women who have a child before the age of 30 have a slightly lower chance of breast cancer. Your breasts complete their development after a first pregnancy, which makes them less sensitive to carcinogens, or cancer-causing substances.
·
Breastfeed
your babies. Research shows that your breast cancer risk is reduced by 7% with
each baby and another 4.3% for each 12 months she breastfeeds. If you have a family history of invasive
premenopausal breast cancer nursing your baby can reduce your risk by as much
as 60%
- Check out your family history. The biggest risk for breast cancer is genetics. If you have certain genetic mutations, called BRCA1 or BRCA2, you're at much higher risk for developing the disease. 20 to 30 % of women with this gene will develop breast cancer by the age of 40 and 50% will by the age of 50. A simple but expensive blood test, $3,100, can tell you if you are a carrier. There are also significant emotional and psychological consequences of testing to consider as well as the risk of discrimination by insurance companies if you do have the genetic abnormality so keep those in mind.
- Consider getting a breast thermography exam which takes a Digital Infrared Image of your breast. It is based on the principle that metabolic activity and vascular circulation in both pre-cancerous tissue and the area surrounding a developing breast cancer is almost always higher than in normal breast tissue. They compare the image from year to year and it can help detect breast cancer much earlier than a traditional mammogram. A thermography exam does not replace a mammogram for those of the appropriate risk group or age range but it can provide even more information about the health of your breast tissue.
DyAnna
Gordon BS,CPM,LDEM is a Southern Utah native, wife and mother of four and a Licensed Certified Professional Midwife
serving Southern Utah and providing homebirth and birth suite services as well
as herbal and nutritional counseling, and breast feeding support.
Subscribe to:
Posts (Atom)



